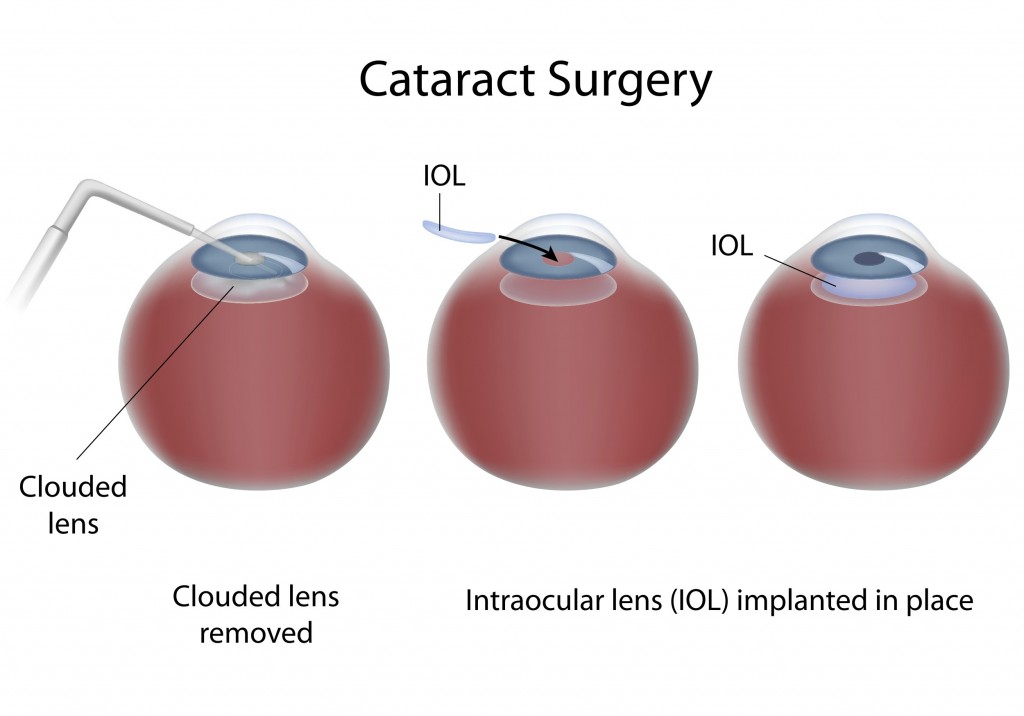
Cataract surgery is a procedure to remove the cloudy lens from the eye and, in most cases, replace it with a new, clear artificial lens called an intraocular lens. Cataract surgery is performed by an eye surgeon (ophthalmologist) on an outpatient basis, which means you don’t have to stay in the hospital after the surgery.
Surgery is recommended for most individuals who have visual symptoms secondary to cataract. When a cataract interferes with the treatment of another eye problem, cataract surgery may be recommended. For example, doctors may recommend cataract surgery if a cataract makes it difficult for your eye doctor to examine the back of your eye to monitor or treat other eye problems such as age-related macular degeneration or diabetic retinopathy.
The mode of surgery can be tailored to individuals based on coexisting medical problems. Cataract surgery is generally performed with minimal sedation and typically takes less than an hour. Therefore the surgery does not put significant strain on the heart or the lungs.
If you have cataracts in both eyes, your doctor usually schedules a second surgery two to four weeks later to remove the cataract in your other eye. This allows time for the first eye to heal before the second eye surgery takes place.
What to expect during cataract surgery?
During cataract surgery, the clouded lens is removed, and a clear artificial lens is usually implanted. In some cases, however, a cataract may be removed without implanting an artificial lens. The most common procedure used for removing cataracts is called phacoemulsification. A small incision is made in the side of the cornea and a tiny instrument that uses high-frequency ultrasound is inserted to break up the center of the cloudy lens and carefully suction it out.
After the cloudy lens has been removed, the surgeon will replace it with an intraocular lens (IOL) implant made of plastic, silicone or acrylic. This new, clear lens allows light to pass through and focus properly on the retina. The IOL requires no care and becomes a permanent part of your eye. In most cases, the IOL is inserted behind the iris, the colored part of your eye, and is called a posterior chamber lens. Sometimes, the IOL must be placed in front of the iris. This is called an anterior chamber lens. When the IOL is in place, the surgeon closes the incision. Stitches may or may not be used.
Intraocular Lens Implants
A variety of IOLs with different features are available. Some IOLs are rigid plastic and implanted through an incision that requires several stitches (sutures) to close. However, many IOLs are flexible, allowing a smaller incision that requires few or no stitches.
Monofocal lens
This common IOL type has been used for several decades.
• Monofocals are set to provide best corrected vision at one distance – near, intermediate or far.
• Most people who choose monofocals have their IOLs set for distance vision and use reading glasses for near activities.
• A person whose IOLs were set to correct near vision would be able to read without glasses but would need glasses to see distant objects clearly.
• Another strategy, called “monovision”, sets one eye for distance vision and the other for near vision. The brain adapts and synthesizes the information from both eyes to provide vision at intermediate distances. Often this reduces the need for reading glasses. Individuals considering monovision should try this technique with contact lenses first to see how well they can adapt to monovision. Those who require crisp, detailed vision may decide monovision is not for them.
Multifocal or accommodative lenses
These IOL types reduce or eliminate the need for glasses or contact lenses.
• In the multifocal type, a series of focal zones or rings is designed into the IOL. Depending on where incoming light focuses through the zones, the person may be able to see both near and distant objects clearly.
• The design of the accommodative lens allows certain eye muscles to move the IOL forward and backward, changing the focus like a natural lens, allowing near and distance vision.
• The ability to read and perform other tasks without glasses varies from person to person but is generally best when multifocal or accommodative IOLs are placed in both eyes.
• It usually takes 6 to 12 weeks after surgery on the second eye for the brain to adapt and vision improvement to be complete with either of these IOL types. Considerations with multifocal or accommodative IOLs
• For many people, these IOL types reduce but do not eliminate the need for glasses or contact lenses.
• Each person’s success with these IOLs may depend on the size of his/her pupils and other eye health factors.
• Side effects such as glare or halos around lights, or decreased contrast sensitivity may occur, especially at night or in dim light. Most people adapt to and are not bothered by these effects, but those who frequently drive at night or need to focus on close-up work may be more satisfied with monofocal IOLs.
Toric IOL for astigmatism
This is a monofocal IOL with astigmatism correction built into the lens.
• Astigmatism: This eye condition distorts or blurs the ability to see both near and distant objects. With astigmatism the cornea (the clear front window of the eye) is not round and smooth (like a basketball), but instead is curved like a football.
• People who want to reduce (or possibly eliminate) the need for eyeglasses may opt for an additional treatment called limbal relaxing incisions, which may be done at the same time as cataract surgery or separately. These small incisions allow the cornea’s shape to be rounder or more symmetrical.
Protective IOL filters
IOLs include filters to protect the eye’s retina from exposure to UV and other potentially damaging light radiation.
Risks of cataract surgery
Complications after cataract surgery are uncommon, and most can be treated successfully.
Cataract surgery risks include:
• Inflammation
• Infection
• Bleeding
• Swelling
• Retinal detachment
• Loss of vision
Your risk of complications is greater if you have another eye disease or a serious medical condition affecting any part of your body. Occasionally, cataract surgery fails to improve vision because of underlying eye damage from other conditions, such as glaucoma or macular degeneration.
After cataract surgery
After cataract surgery, expect your vision to begin improving within a few days. Your vision may be blurry at first as your eye heals and adjusts.
You’ll usually see your eye doctor a day or two after your surgery, the following week, and then again after about a month to monitor healing.
It’s normal to feel itching and mild discomfort for a couple of days after surgery. Avoid rubbing or pushing on your eye. Your doctor may ask you to wear an eye patch or protective shield the day of surgery.
Your doctor may prescribe eyedrops or other medication to prevent infection, reduce inflammation and control eye pressure. After a couple of days, most of the discomfort should disappear. Often, complete healing occurs within eight weeks.
Contact your doctor immediately if you experience any of the following:
• Vision loss
• Pain that persists despite the use of over-the-counter pain medications
• Increased eye redness
• Light flashes or multiple new spots (floaters) in front of your eye
• Nausea, vomiting or excessive coughing
Most people need glasses, at least some of the time, after cataract surgery. Your doctor will let you know when your eyes have healed enough for you to get a final prescription for eyeglasses.
Cataract surgery successfully restores vision in the majority of people who have the procedure.
People who have had cataract surgery may develop a common complication known as posterior capsule opacification (PCO), or secondary cataract. This happens when the back of the lens capsule — the part of the lens that wasn’t removed during surgery and that now supports the lens implant — becomes cloudy and impairs your vision.
PCO is treated with a painless, five-minute outpatient procedure called yttrium-aluminum-garnet (YAG) laser capsulotomy. In YAG laser capsulotomy, a laser beam is used to make a small opening in the clouded capsule to provide a clear path through which the light can pass.